In recent years, Vitamin D deficiency has emerged as one of the most unseen health challenges in both developing and developed countries. Often known as the “sunshine vitamin”, vitamin D plays an important role in maintaining bone health, regulating immunity, and supporting different physical functions. Despite much sunlight in countries such as India, the surprising number of people in all age groups suffer from insufficient vitamin D levels – a contradiction that needs deeper examination.
Why Vitamin D Matters More Than You Think!
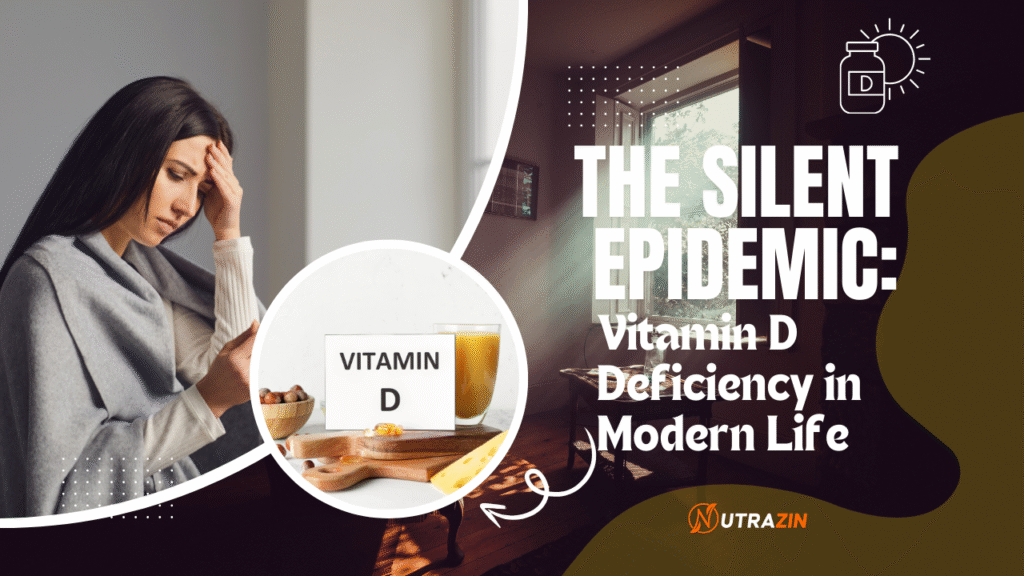
Vitamin D is unique among essential nutrients. Unlike other vitamins that are mainly achieved through food, Vitamin D can be synthesized by the human body when the skin is exposed to sunlight, especially ultraviolet B (UVB) rays. When produced or swallowed, it undergoes conversion to the liver and kidney to become active and functional.
This vitamin is central to the absorption of calcium and phosphorus – two large minerals responsible for bone strength. Without enough Vitamin D, even a calcium-rich diet cannot stop osteoporosis or rickets. But the scope of its influence goes far beyond skeletal health. It also plays a role in:
- Supporting immune system responses
- Enhancing mood and combating depression
- Reducing inflammation
- Modulating heart and metabolic functions
Despite these well-established benefits, the modern lifestyle has created many obstacles to maintaining the level of optimal vitamin D.
Causes Behind Widespread Deficiency:
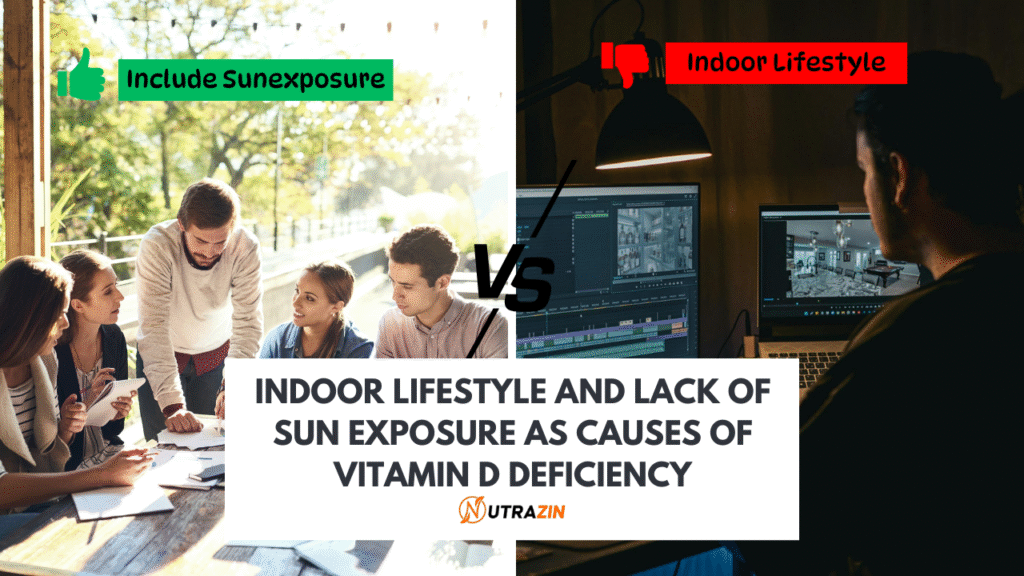
Vitamin D deficiency is not due to the same reason; This is the result of a combination of factors created in urban and semi-urban life. The most prominent of these is the lack of sufficient sun exposure.
At a time when people spend most of the day indoors – whether in offices, schools, or home – direct contact with sunlight has significantly slowed down. Even when out, sunscreen, air pollution, and clothing that covers most of the body limit the skin’s ability to synthesize Vitamin D in the skin efficiently.
Dietary habits increase the problem further. Natural food sources that are rich in vitamin D are relatively limited and include fatty fish (e.g. salmon and mackerel), cod liver oil, egg yolk, and strong dairy products. These are either low segments or inaccessible to low segments, especially in lower-income or vegetarian communities.
In addition, some medical and physical conditions may prevent the absorption or activation of vitamin D. These include:
- Malabsorption disorders (e.g., celiac disease, Crohn’s disease)
- Chronic kidney or liver disease
- Obesity (where Vitamin D gets stored in fat and becomes less bioavailable)
- Advancing age, which reduces the skin’s efficiency in producing Vitamin D
Recognizing the Subtle Symptoms
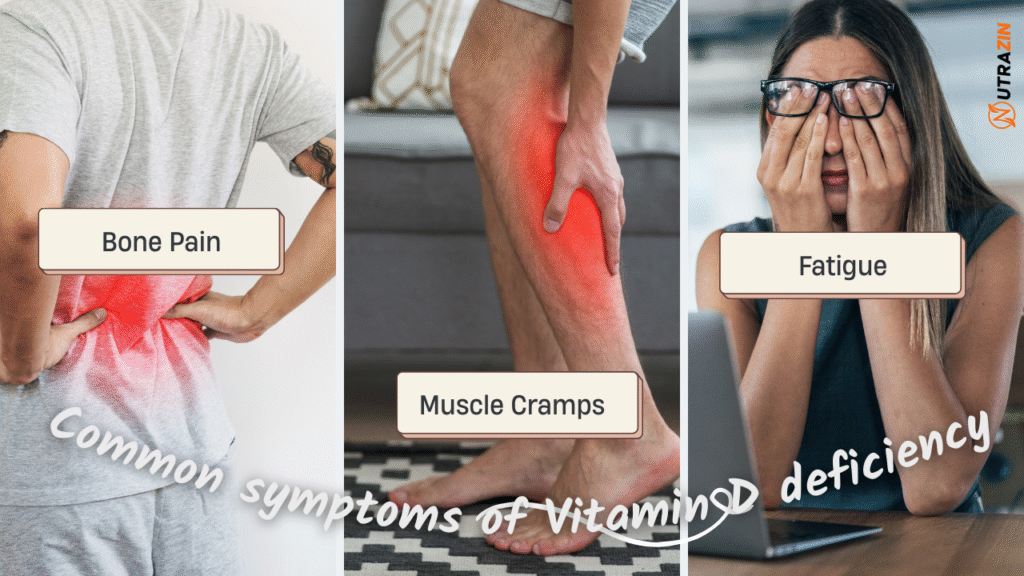
Vitamin D deficiency makes the defect particularly dangerous and has a tendency to develop slowly and quietly. Many people remain unaware for several months or years, attributed to vague symptoms of stress, age, or general fatigue.
Some often reported symptoms include:
- Constant fatigue and low energy
- Generalized aches or lower back pain
- Muscle cramps
- Increased sensitivity to infection
- Depressed mood or irritability
- Delayed wound healing
- Hair thinning
In more advanced cases, especially in children, deficiencies can cause rickets, weak bones, and skeletal deformities. In adults, osteomalacia (soft bones) or osteoporosis (brittle bones) can significantly increase the risk of fracture and mobility problems.
Who is at high risk?
While vitamin D deficiency can affect anyone, some groups are more weak than others. This includes:
- Old adults, especially those over 60
- Pregnant and breastfeeding women
- Infants who are exclusively breastfed without supplementation
- For people with dark skin colors, melanin reduces vitamin D synthesis
- People who come into contact with the limited sun due to clothing, lifestyle, or place
Identifying these high-risk groups is necessary for initial screening and timely intervention.
Diagnosis and monitoring
The most reliable method of assessing the condition of vitamin D is a blood test that measures serum 25-hydroxyvitamin D levels. According to global health guidelines:
- The level below 20 ng/mL indicates a deficiency
- The level between 20-30 ng/mL is considered insufficient
- The optimal level is 30-100 ng/mL
If the deficiency is detected, doctors may recommend further tests, especially if there is talk of bone health. These may include bone mineral density scanning or calcium level assessment.
Addressing the deficiency: What can be done?
The good news is that vitamin D deficiency is both preventable and treatable. It requires a combination of lifestyle changes, dietary improvements, and supplements when needed.
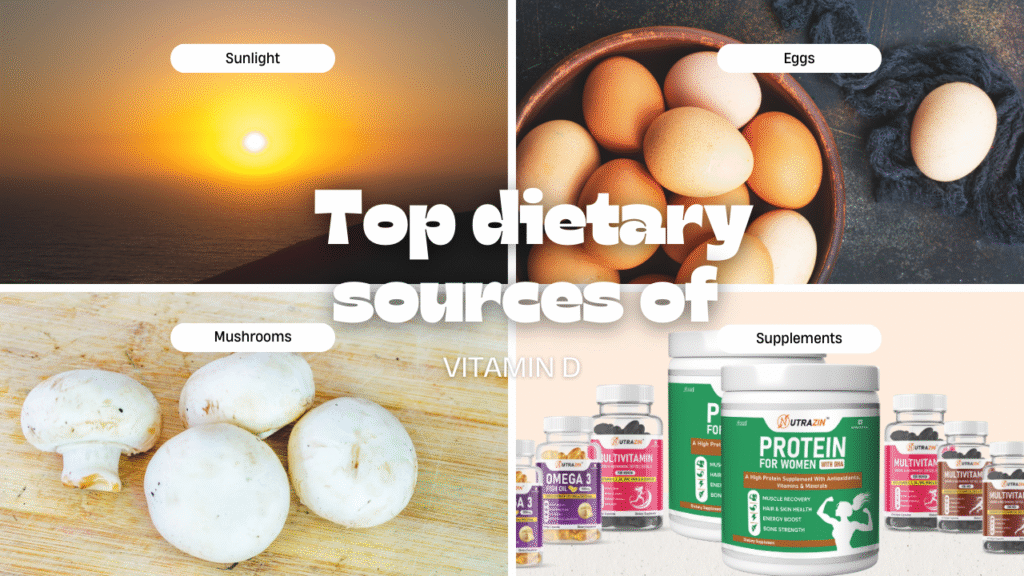
Sunlight Exposure:
Encouraging safe, regular performance for sunlight is the most natural and cost-effective approach. Ideally, spending 15-30 minutes in the sunlight – without sunscreen – on the face, hands, and feet, can help promote the level of vitamin D at least 2-3 times a week. UVB is the most effective window for absorption (10 to 15).
However, people living in polluted or cold areas may not have an advantage, making dietary sources and everything more important.
Improvement of dietary intake:
Although food alone cannot meet daily vitamin D requirements for most people, including some items, can help maintain levels:
- Fatty fish (e.g. salmon, sardines, and tuna)
- Egg yolk
- Fortified milk and orange juice
- Mushrooms exposed to sunlight
- Cheese and fortified Plant-based Milk Options
In countries where fortifications are not widespread, awareness and access to such products require significant improvement.
Supplements:
When the sun’s contact and diet decrease, a dose of vitamin D is necessary. Depending on the severity of the deficiency, the doctor may prescribe:
- Maintenance doses: typically 800–2000 IU per day
- Therapeutic doses: such as 50,000 IU weekly for 6–8 weeks
These supplements are usually safe when used during medical supervision. However, critical use can cause vitamin D toxicity, resulting in nausea, hypercalcemia, kidney damage, or confusion.
Immune Connection: A New Perspective
The COVID-19 epidemic focused on the role of vitamin D in supporting immune function. Overview studies suggested that when infected, individuals with sufficient vitamin D levels had better results. Although more research is needed to establish work-promoting, these conclusions emphasize the widespread importance of maintaining optimal vitamin D for general flexibility.
Public health implications and awareness
Despite the growing body of scientific evidence, public awareness of vitamin D deficiency is low. Many people continue to believe that living in a sunny country automatically protects them, or that their routine diet suffices. This misconception can be dangerous, especially for a vulnerable population.
There is a pressing need for health learning campaigns, social level screening programs to promote vitamin D-rich diets, regular outdoor activity and supplements.
Conclusion
Vitamin D deficiency may not cause immediate alarm, but its long-term effects on bone health, immunity, and quality of life are deep. In a world where sunlight is often traded for screen, and natural habits cope with artificial routines, we must remember that some of the most important nutrients cannot be replaced by convenience. A conscious return to a healthy lifestyle – with a little more time in the sun, a more thoughtful diet, and proactive healthcare – can help us reclaim our health from this quiet epidemic.